Abstract
We present a rare case of traumatic ureteric artery bleeding successfully treated with transcatheter arterial embolization. A 65-year-old male with blunt abdominal trauma and hypotension was found to have a left retroperitoneal hematoma with active extravasation on CT. Initial angiography showed no visible bleeding; however, cone-beam CT revealed active hemorrhage from a ureteric artery displaced by the hematoma. Selective embolization using n-butyl cyanoacrylate and ethiodized oil was performed, resulting in hemodynamic stabilization. Follow-up imaging demonstrated resolution of bleeding and positional change of the ureteric artery as the hematoma resolved. This case highlights the diagnostic value of cone-beam CT and the importance of considering ureteric artery injury in cases of unexplained retroperitoneal hemorrhage.
-
Keywords: Wounds and injuries; Wounds, nonpenetrating; Embolization; Therapeutic; Ureter
Introduction
Traumatic retroperitoneal hematoma occurs in approximately 67-80% of blunt injuries, and it has been identified in approximately 12% of hemodynamically stable patients with abdominal trauma [
1]. Retroperitoneal hemorrhage is often asymptomatic, which may lead to it being overlooked by clinicians, potentially resulting in significant morbidity and mortality. Although there have been reports of transcatheter arterial embolization (TAE) for retroperitoneal hemorrhage involving the lumbar or iliolumbar arteries, no cases have been reported involving traumatic bleeding from the ureteric artery.
Here, we present a case report of successful TAE for traumatic ureteric artery bleeding, accompanied by detailed imaging findings.
Case Report
A 65-year-old male pedestrian presented to the level I trauma center emergency department following a motor vehicle collision. On arrival, his blood pressure was 60/40 mmHg and his heart rate was 120 beats per minute. Laboratory evaluation revealed a serum hemoglobin level of 12.6 g/dL, a platelet count of 237,000/mm
3, and an INR of 1.02. Contrast-enhanced thoracoabdominal CT, performed to identify possible bleeding sources, demonstrated a left retroperitoneal hematoma with active extravasation (
Fig. 1). Associated fractures were noted in the left iliac bone at the anterior superior iliac spine and the left transverse process of L5. There was no evidence of hematuria or hydronephrosis.
An emergent angiographic evaluation and embolization were requested to the interventional radiology team. Selective angiography of the arteries suspected to be potential bleeders—the adjacent left lumbar arteries, left iliolumbar artery, and left deep circumflex iliac artery—performed with hand injection of contrast medium, revealed no visible contrast extravasation; however, empirical embolization of these arteries was performed using a mixture of n-butyl cyanoacrylate (NBCA) (Histoacryl; B Braun, Rubi, Spain) and ethiodized oil (Lipiodol Ultra; Guerbet Pharmaceuticals, Paris, France) based on the presumption that bleeding may have already ceased. NBCA, a permanent embolic agent, was chosen due to concern that recanalization of the arteries could lead to rebleeding once hypovolemia was corrected and blood pressure increased. As it was considered that all potentially bleeding arteries had been embolized and the patient’s vital signs had stabilized, aortography was not performed.
Seven hours after the empirical embolization procedure, the patient remained hypotensive despite intravenous hydration and blood transfusion. Repeat contrast-enhanced CT demonstrated an increase in the size of the left retroperitoneal hematoma with persistent active bleeding. Selective angiography of the infrarenal abdominal aorta branches—including the left renal and renal capsular arteries, left testicular artery, and inferior mesenteric artery—showed no evidence of hemorrhage. As bleeding was presumed to originate from a fine arterial branch not visualized on selective angiography, a 5-Fr diagnostic catheter (pigtail catheter; Jungsung Medical, Seoul, Korea) was positioned in the suprarenal abdominal aorta, and cone-beam CT was performed using a 7 mL/sec injection of a total of 70 mL of contrast (Visipaque 270mg I/ml, GE Healthcare, Shanghai, China).
Axial cone-beam CT images revealed a thin artery arising at the 12 o’clock position from the infrarenal aorta, which coursed leftward toward the left ureter, made an L-shaped bend, and descended, with active bleeding observed (
Fig. 2). Based on these findings, selective catheterization of this artery was achieved using the 5-Fr diagnostic catheter (RH; Jungsung Medical, Seoul, Korea) and a 1.5-Fr microcatheter (Veloute Ultra, Asahi Intecc, Nagoya, Japan). Embolization was then performed using a 1:4 mixture of NBCA and ethiodized oil.
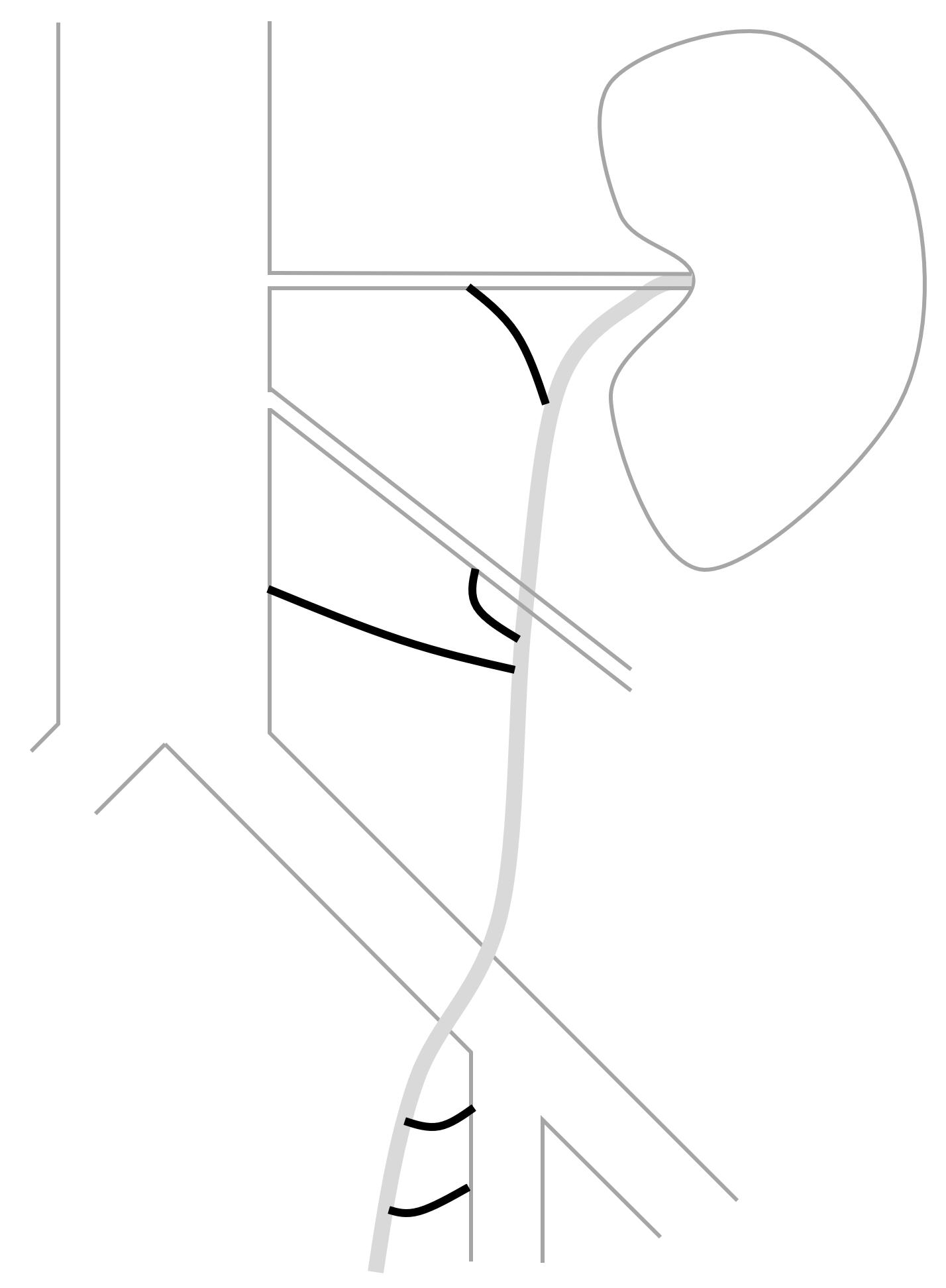
Following the procedure, the patient’s blood pressure normalized. One month later, a delayed-phase abdominopelvic CT demonstrated embolic material tracking along the course of the left ureter. Notably, when the retroperitoneal hematoma was large, the left ureteric artery appeared to originate at the 12 o’clock position; however, as the hematoma decreased, the origin of the artery was observed to shift to the 3 o’clock position (
Fig. 3). During the three-month follow-up period, the patient developed distal ureteral stenosis, which was suspected to result from the ureteric artery embolization. The patient is currently under urological outpatient follow-up with a double-J stent in situ.
Discussion
Traumatic or iatrogenic injury to the ureteric artery is rare. Reports of TAE for such cases are limited to a few case studies; postoperative iatrogenic ureteric artery injury [
2,
3], and ureteric artery bleeding caused by retroperitoneal invasion due to pelvic lymph node metastasis from gastric cancer [
4].
The upper (abdominal) segment of the ureter is primarily supplied by fine ureteric branches originating from the main renal artery. Less commonly, arterial supply may also arise from the abdominal aorta or the gonadal arteries. These vessels approach the ureter medially and bifurcate into ascending and descending branches, forming a longitudinal anastomosis along the ureteral wall [
5] (
Fig. 4). Anatomically, the ureteric artery typically originates laterally from the abdominal aorta. However, in the present case, it appeared to originate anteriorly due to displacement caused by a surrounding hematoma. On follow-up computed tomography, after resolution of the hematoma, the artery was again visualized as originating laterally. This case underscores that an exclusive assumption of a lateral origin from the abdominal aorta may impede the precise identification of the ureteric artery in certain clinical contexts.
In summary, we successfully performed selective embolization of the left ureteric artery, which was the source of bleeding due to traumatic injury, with the aid of cone-beam CT in identifying its origin. During the procedure, possible displacement of surrounding organs and arteries by the hematoma should be considered, and isolated bleeding from fine arteries such as the ureteric artery should be recognized.
Conflict of interest
All authors have no conflicts of interest to declare.
Funding
None.
Acknowledgments
None.
Author contributions
All the work was done by Suyoung Park.
Fig. 1.Preprocedural contrast-enhanced abdominopelvic CT reveals a left retroperitoneal hematoma with associated contrast media extravasation (asterisk).

Fig. 2.Axial and coronal cone-beam CT images as well as angiographic image, obtained during the procedure, demonstrate a bleeding left ureteric artery (arrows) originating from the abdominal aorta in the 12 o’clock direction and coursing posterolaterally to the left before sharply angling into an L-shaped configuration.

Fig. 3.Follow-up CT after hematoma reduction shows the embolized left ureteric artery (arrow) as a hyperdense structure due to the presence of embolic materials. With the hematoma resolved, the artery appears to originate laterally.

Fig. 4.In this schematic drawing of the segmental arterial supply to the ureteric artery, the supplying arteries are depicted as thick black lines: from top to bottom, the renal artery branch, gonadal artery branch, aortic branch, and multiple branches of the internal iliac artery.
References
- 1. Mondie C, Maguire NJ, Rentea RM. Retroperitoneal Hematoma. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2025.
- 2. Maleux G, Stockx L, Wilms G, Bogaert G, Marchal G. Postoperative retroperitoneal hemorrhage due to a bleeding ureteric artery: treatment by transcatheter embolization. Eur Radiol. 2001;11:34-36.
- 3. Kase DJ, Crystal KS, Naidich JB, Badillo FL, Waldbaum RS. Embolization to control iatrogenic ureteral hemorrhage: a case report. J Urol. 1994;151:420-421.
- 4. Saiga A, Aramaki T, Sato R, Asahara K, Goto H. Embolization of pseudoaneurysms in the ureteral branch of the renal artery. CVIR Endovasc. 2023;6:51.
- 5. Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, Wein AJ. Arteries, veins, and lymphatic drainage of the ureters. Campbell-Walsh-Wein Urology. 12th. Philadelphia, PA: Elsevier, 2021;1874.
Citations
Citations to this article as recorded by